Laser Therapy for Toenail Fungus

Toenail fungus, medically known as onychomycosis, is a condition that affects countless individuals, causing nails to become discolored, brittle, and thickened. Traditional treatment methods, such as oral medications or topical ointments, often yield mixed results and can take months to show improvement. This is where laser therapy, a relatively new approach, comes into play. Laser therapy for toenail fungus, also referred to as laser mycotic nail treatment, involves the use of a concentrated beam of light to target and destroy the fungal organisms that are infecting the nail. The laser's energy penetrates the nail, without causing harm to the surrounding tissue, to eliminate the fungus at its source. This innovative approach boasts several advantages, including minimal discomfort, no need for anesthesia, and typically shorter treatment times compared with traditional methods. However, it is important to note that laser therapy is not a guaranteed cure and may require multiple sessions for the best results. While promising, its effectiveness varies from person to person. If you have toenail fungus, it is suggested that you visit a podiatrist who can determine if laser therapy is correct for you.
Laser treatment can be an effective way to get rid of toenail fungus. If you have any questions about laser treatment, consult with Amir Shalev, DPM from Complete Foot & Ankle Care. Our doctor will assess your condition and provide you with quality treatment for fungal nails.
What Are Toenail Fungal Infections?
Onychomycosis, or fungal infection of the nail, is a relatively common and non-serious condition. Around 10 percent of U.S. citizens are afflicted with fungal nails. Common forms of fungus that infect the nail include dermatophytes, yeasts, and molds.
Symptoms of Toenail Fungal Infections Include:
- Nail thickening
- Brittleness of the nail
- Discoloration of the nail
Diagnosis for Fungal Nails
Fungal infections are diagnosed by fungal culture and microscopy. This will rule out any other conditions such as nail trauma, psoriasis, lichen planus, and onychogryphosis.
What Is Laser Treatment?
Laser treatment is a non-invasive, safe, quick, and painless procedure that uses the heat from a laser to kill fungus in the nail. Each infected nail is targeted with a laser for several minutes. The treatment is usually utilized several different times over a select period. During this time, a podiatrist will keep an eye on the infection.
If you have any questions, please feel free to contact our office located in Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Laser Treatment for Fungal Nails
A new treatment for fungal nails, or onychomycosis, which has grown in popularity in recent years, is laser treatment. Laser treatment involves the use of a laser that kills fungus in the toenail with heat. Laser therapy causes no side effects and does not affect nearby healthy tissue.
Toenail fungus afflicts almost 10 percent of the U.S. population and is more common among the elderly. The most common symptom of toenail fungus is the discoloration and thickening of the nail. The nail can also become brittle and a foul smell may be produced. In rare cases, pain might be present. While it is not a serious condition, it can lead to a perception of disgust amongst those it affects. There are several different fungi that cause fungal infections. These include dermatophyte, yeast, and mold. The most common of these is dermatophyte.
Diagnosis for fungal nails involves a podiatrist utilizing microscopy and fungal cultures. This will allow the doctor to determine whether it is a fungus or another condition, such as lichen planus, psoriasis, nail damage, and onychogryphosis.
Fungus in the nails can be hard to get rid of with over-the-counter drugs. This is due to the nail being hard and protective, with fungus able to slip between the nail bed and plate. Furthermore the slow growth of the nail increases the difficulty of fungus going away. Laser treatment seeks to get around this by directly penetrating through the nail and killing the fungus. The laser is used on each infected nail for a couple of minutes. Patients then typically return several weeks or months later for another laser treatment. During this time the podiatrist will routinely observe the foot and infection. It is also recommended to wear clean socks and shoes and allow the feet to dry and breathe to prevent toenail fungus.
Laser treatment is still a relatively new treatment and not all podiatrists have laser machines. Ask your podiatrist if they do laser treatment for toenail fungus and if it is right for you.
Definition and Reasons for Developing Hammertoe

Hammertoe, a relatively common foot condition, is often the source of discomfort and inconvenience for many individuals. This deformity occurs when the middle joint of one or more of your smaller toes becomes bent and stuck in an abnormal position. The affected toes often resemble the shape of a hammer, hence the name. Hammertoes can develop for a variety of reasons, including genetics, foot structure, or wearing ill-fitting shoes. High heels and shoes that squeeze the toes together can exacerbate the problem. Hammertoes can lead to pain, corns, calluses, and difficulty finding comfortable footwear. While the condition can be hereditary, early intervention through wearing proper footwear and certain medical treatment can help prevent or alleviate the discomfort associated with hammertoes, allowing individuals to maintain healthier and happier feet. If you are afflicted with hammertoe, it is strongly suggested that you are under the care of a podiatrist who can guide you toward effective relief options.
Hammertoes can be a painful condition to live with. For more information, contact Amir Shalev, DPM of Complete Foot & Ankle Care. Our doctor will answer any of your foot- and ankle-related questions.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the muscles, tendons, or ligaments that normally hold the toe straight. It can be caused by the type of shoes you wear, your foot structure, trauma, and certain disease processes.
Symptoms
- Painful and/or difficult toe movement
- Swelling
- Joint stiffness
- Calluses/Corns
- Physical deformity
Risk Factors
- Age – The risk of hammertoe increases with age
- Sex – Women are more likely to have hammertoe compared to men
- Toe Length – You are more likely to develop hammertoe if your second toe is longer than your big toe
- Certain Diseases – Arthritis and diabetes may make you more likely to develop hammertoe
Treatment
If you have hammertoe, you should change into a more comfortable shoe that provides enough room for your toes. Exercises such as picking up marbles may strengthen and stretch your toe muscles. Nevertheless, it is important to seek assistance from a podiatrist in order to determine the severity of your hammertoe and see which treatment option will work best for you.
If you have any questions, please feel free to contact our office located in Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the tendons, muscles, or ligaments that are responsible for holding the toes in their normal position. This condition may be caused by poor footwear, foot structure, trauma, and disease. The most common solution for hammertoe is to relieve the pain by changing your footwear and wearing orthotics. In severe cases, surgery may be required.
The shoes that are most likely to cause hammertoe are high heeled shoes or shoes that are too tight in the toe box. Tight shoes will force your toes to crowd together in a curled position. This position will likely continue when you take your shoes off. Another cause is trauma. When you stub your toe, you are increasing the chance that you will develop hammertoe.
There are risk factors that may make you more likely to develop this condition. Women are more likely to have the condition compared to men, and it is also more likely to appear in those who are older in age.
Many different foot problems can be avoided by wearing shoes that have adjustability, adequate toe room, and low heels. Furthermore, if you want to buy new shoes, you should look to purchase them at the end of the day and make sure you know your correct size. The importance of buying shoes at the end of the day is that your feet swell as the day progresses. You should also ensure that you are wearing your correct size because your shoe size may change as you grow older.
To diagnose someone with hammertoe, your podiatrist will need to conduct a thorough examination of your foot. Your doctor may even order an x-ray to evaluate the bones and joints of your feet and toes.
If you have hammertoe, your podiatrist may recommend that you wear shoes that fit you better along with inserts to place inside them. Additionally, he or she may suggest special exercises for you to perform to stretch your toes. One helpful exercise it to pick up marbles with your feet or crumple a towel with your toes.
Prior to meeting with your podiatrist, it will be helpful to make a list of all the symptoms you are experiencing. You should also make a note of medications you are taking and important personal information about your medical history.
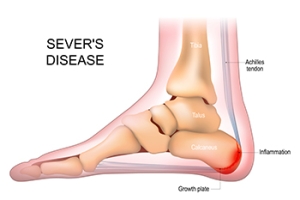
Causes and Treatment Options for Sever’s Disease
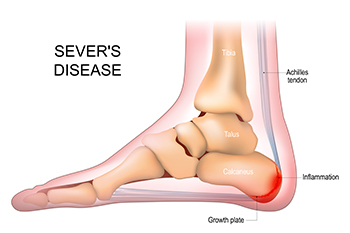
Sever's disease, also known as calcaneal apophysitis, is a common heel condition affecting children during growth spurts. The primary cause lies in the heel bone's growth plate, which is still developing and can become inflamed due to repetitive stress and tension. This often occurs in active children involved in sports or activities that involve a lot of running and jumping. The growth plate is more vulnerable during this period of rapid growth, making it susceptible to injury and irritation. The good news is that Sever's disease is manageable and typically resolves on its own as the growth plate solidifies. Treatment involves rest, modifying activities, stretching exercises, and wearing supportive footwear to alleviate symptoms and promote healing. If your active child has heel pain, which is a common symptom of Sever’s disease, it is suggested that you consult a podiatrist. This type of doctor can offer tailored treatment options for this condition.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see Amir Shalev, DPM from Complete Foot & Ankle Care. Our doctor can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our office located in Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.
Sever's Disease
Sever’s disease, also known as calcaneal apophysitis is a common bone disorder that occurs during childhood. The disease is defined as an inflammation of the growth plate in the heel. When a child has a growth spurt, his heel bone grows faster than the muscles, tendons, and ligaments in his leg. This disease is a result of overuse. The people who are most likely to be affected by this disease are children who are in a growth spurt, especially boys who are from the ages of 5 to 13 years old. 60% of children with Sever’s disease have both heels involved.
Symptoms of this disease are heel pain that intensifies during running and jumping activities. The pain is typically localized to the posterior part of the heel. Symptoms may be severe, and they can easily interfere with daily activities. Children who play soccer, baseball, and basketball are more likely to develop Sever’s disease.
Your doctor will diagnose your child based on his or her symptoms, x-rays are generally not helpful in diagnosing this disease. Your doctor may examine both heels and ask your child questions about his or her activity level in sports. Your doctor may then use the squeeze test on your child’s heel to see if there is any pain. Nevertheless, some doctors might still use x-rays to rule out any other issues such as fractures, infections, and tumors.
Sever’s disease can be prevented by maintaining good flexibility while your child is growing. Another prevention method is to wear good-quality shoes that have firm support and a shock-absorbent sole. Sever’s disease can be treated by ceasing any activity that causes heel pain. You should apply ice to the injured heel for 20 minutes 3 times a day. Additionally, orthotics should be used for children who have high arches, flat feet, or bowed legs.
If you suspect your child has Sever’s disease, you should make an appointment with your podiatrist to have his or her foot examined. Your doctor may recommend nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen to relieve pain. In more severe cases, your child may need a cast to rest his or her heel. Fortunately, Sever’s disease does not cause long-term foot problems. After treatment, your child should start to feel better within two weeks to two months.
Achilles Tendon Ruptures

Achilles tendon ruptures are serious injuries often resulting from participating in intense physical activities such as running or sports involving quick turns and stops. If you experience a sharp pain accompanied by a popping sound in the back of your leg, it may indicate a tear in your Achilles tendon. Immediate diagnosis by a podiatrist, done typically through a physical examination and possibly an MRI, is crucial to determine the severity of the tear. Partial tears may require immobilization using a boot or splint, allowing the tendon to naturally heal over the course of approximately six weeks. Complete ruptures, however, often necessitate surgical intervention. Post-injury care includes elevation of the leg and pain medication. If you feel you may have ruptured your Achilles tendon, it is suggested that you make an appointment with a podiatrist for a prompt diagnosis and treatment.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Amir Shalev, DPM of Complete Foot & Ankle Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Las Vegas, NV . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
The Causes, Types, and Treatments of Achilles Tendon Injuries
Tendons are fibrous tissues that connect muscles with bone. The Achilles tendon is the largest tendon in the body. It connects the calf muscles at the back of the leg with the heel, and facilitates movements such as jumping, running, and walking.
Because the Achilles tendon is engaged so frequently and bears a great deal of pressure and stress throughout the day, it can become injured. Achilles tendon injuries cause the tissue to become irritated, inflamed, and swollen. Pain can come on gradually or be immediate, and will vary from mild to severe depending upon the injury. Where the pain occurs will vary as well, from just above the heel up through the back of the leg. There may also be stiffness in the tendon.
Achilles tendon injuries can often be caused by repetitive stress. They may also occur while running, playing tennis, gymnastics, football, basketball, dancing, soccer, baseball or other sports that require speeding up, slowing down, or pivoting quickly. Wearing high heels, falling from an elevation, stepping in a hole, having flat feet, bone spurs, tight leg muscles or tendons, wearing improper athletic shoes, exercising on uneven surfaces, or starting a new type of exercise can also cause Achilles tendon injuries.
The two most common Achilles tendon injuries are tendonitis and ruptures. Tendonitis causes painful inflammation and can occur in different parts of the tendon. Non-insertional Achilles tendonitis occurs when the fibers in middle of the tendon begin to break down, thicken, and swell. This condition typically affects younger, more active adults. Insertional Achilles tendonitis occurs where the tendon inserts into the heel bone. It is common for bone spurs to form with this type of injury. This condition can affect people of any age and level of activity.
Achilles tendon ruptures are a tear in the tendon. These breaks may be partial or complete. There may be an audible popping noise at the moment of injury and the pain will be sudden and severe.
An Achilles tendon injury can be diagnosed by your podiatrist after they examine you, check your range of motion, and possibly perform a calf squeeze test or review an X-ray or MRI. Depending on the type and severity of your injury, your podiatrist may treat your condition with rest/ice/compression/elevation (RICE), nonsteroidal anti-inflammatory medications, heel lifts, and stretching and strengthening exercises. If you have torn your Achilles tendon, treatment may include physical therapy, ultrasound, shockwave therapy, or possibly even surgery.
Recognizing the Signs and Finding Relief for a Broken Toe

A broken toe can happen to anyone, whether it is from a sudden accident or a simple misstep. The first step in treating a broken toe is recognizing the signs. Pain, swelling, bruising, and difficulty in moving the toe are common indicators. If you suspect a break, it is essential to seek medical attention promptly. To confirm the broken toe, a diagnosis is often needed by having an X-ray taken. In the meantime, you can take some steps to alleviate discomfort. Resting the affected foot and elevating it may help to reduce swelling. Immobilize the toe by buddy-taping it to an adjacent healthy toe, which can provide support and stability during the healing process. Taking over-the-counter pain relievers can help to manage pain, and it is helpful to avoid putting weight on the injured toe. If the fracture is severe or displaced, the toe may need to be reset or placed in a splint. Healing a broken toe takes time, so it is advised to be patient and take good care of your injured toe. If you have broken your toe, it is suggested that you visit a podiatrist who can effectively diagnose and treat this injury.
A broken toe can be very painful and lead to complications if not properly fixed. If you have any concerns about your feet, contact Amir Shalev, DPM from Complete Foot & Ankle Care. Our doctor will treat your foot and ankle needs.
What to Know About a Broken Toe
Although most people try to avoid foot trauma such as banging, stubbing, or dropping heavy objects on their feet, the unfortunate fact is that it is a common occurrence. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break (fracture).
Symptoms of a Broken Toe
- Throbbing pain
- Swelling
- Bruising on the skin and toenail
- The inability to move the toe
- Toe appears crooked or disfigured
- Tingling or numbness in the toe
Generally, it is best to stay off of the injured toe with the affected foot elevated.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery. Due to its position and the pressure it endures with daily activity, future complications can occur if the big toe is not properly treated.
If you have any questions please feel free to contact our office located in Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.